Overview

?Pes Planus? is the medical term for flat feet. It comes from Latin: Pes = foot and Planus = plain, level ground. Very few people suffer from this condition, as a true flat foot is very rare. Less than 5% of the population has flat feet. The majority of the Australian population, however, has fallen arches (an estimated 60-70% of the population) known in the medical profession as ?excess pronation? or over-pronation. Over-pronation means the foot and ankle tend to roll inwards and the arch collapses with weight-bearing. This is a quite a destructive position for the foot to function in and may cause a wide variety of foot, leg and lower back conditions.
Causes
Flat feet in adults can arise from a variety of causes. Here are the most common. An abnormality that is present from birth, stretched or torn tendons, damage or inflammation of the posterior tibial tendon (PTT), which connects from your lower leg, along your ankle, to the middle of the arch, broken or dislocated bones. Some health conditions, such as rheumatoid arthritis, Nerve problems. Other factors that can increase your risk include obesity, diabetes, ageing and Pregnancy.
Symptoms
The primary symptom of flatfeet is the absence of an arch upon standing. Additional signs of flatfeet include the following. Foot pain. Pain or weakness in the lower legs. Pain or swelling on the inside of the ankle. Uneven shoe wear. While most cases of flatfeet do not cause problems, complications can sometimes occur. Complications include the following, bunions and calluses, inability to walk or run normally, inflammation and pain in the bottom of the foot (plantar fasciitis), tendonitis in the Achilles heel and other ligaments, pain in the ankles, knees, and hips due to improper alignment, shin splints, stress fractures in the lower legs.
Diagnosis
People who have flat feet without signs or symptoms that bother them do not generally have to see a doctor or podiatrist about them. However, if any of the following occur, you should see your GP or a podiatrist. The fallen arches (flat feet) have developed recently. You experience pain in your feet, ankles or lower limbs. Your unpleasant symptoms do not improve with supportive, well-fitted shoes. Either or both feet are becoming flatter. Your feet feel rigid (stiff). Your feet feel heavy and unwieldy. Most qualified health care professionals can diagnose flat feet just by watching the patient stand, walk and examining his/her feet. A doctor will also look at the patient's medical history. The feet will be observed from the front and back. The patient may be asked to stand on tip-toe while the doctor examines the shape and functioning of each foot. In some cases the physician may order an X-ray, CT (computed tomography) scan, or MRI (magnetic resonance imaging) scan.
Non Surgical Treatment
If you have flat feet and foot pain, especially if one foot is flatter than the other, you should have an evaluation by an orthopedic surgeon . You may have a problem with the posterior tibial tendon , the main tendon that supports the arch. Factors that can contribute to this problem are obesity, diabetes , high blood pressure , certain types of arthritis and athletic overuse. In some cases a shoe insert/orthotic can be used to alleviate the symptoms of flat feet.
Surgical Treatment

This is rare and usually only offered if patients have significant abnormalities in their bones or muscles. Treatments include joint fusion, reshaping the bones in the foot, and occasionally moving around tendons in the foot to help balance out the stresses (called tendon transfer).
Prevention
oll away pain. If you're feeling pain in the arch area, you can get some relief by massaging the bottom of your foot. A regular massage while you're watching TV can do wonders" Stretch out. Doing the same type of stretching exercises that runners do in their warm-up can help reduce arch pain caused by a tight heel cord. One of the best exercises is to stand about three feet from a wall and place your hands on the wall. Leaning toward the wall, bring one foot forward and bend the knee so that the calf muscles of the other leg stretch. Then switch legs. Stretching is particularly important for women who spend all week in heels and then wear exercise shoes or sneakers on weekends. Get measured each time you buy new shoes. Don't assume that since you always wore a particular size, you always will. Too many people try to squeeze into their 'regular' shoe size and wind up with serious foot problems or sores on their feet. When your arch is falling, your feet may get longer or wider and you may or may not feel pain, so getting your foot measured each time you buy shoes is a good indicator of your arch's degeneration. Examine your shoes. If the heel is worn down, replace it. But if the back portion of the shoe is distorted or bent to one side, get yourself into a new pair of supportive shoes like those made specifically for walking. That's because flat feet can affect your walking stride, and failing to replace worn shoes may lead to knee or hip pain.

?Pes Planus? is the medical term for flat feet. It comes from Latin: Pes = foot and Planus = plain, level ground. Very few people suffer from this condition, as a true flat foot is very rare. Less than 5% of the population has flat feet. The majority of the Australian population, however, has fallen arches (an estimated 60-70% of the population) known in the medical profession as ?excess pronation? or over-pronation. Over-pronation means the foot and ankle tend to roll inwards and the arch collapses with weight-bearing. This is a quite a destructive position for the foot to function in and may cause a wide variety of foot, leg and lower back conditions.
Causes
Flat feet in adults can arise from a variety of causes. Here are the most common. An abnormality that is present from birth, stretched or torn tendons, damage or inflammation of the posterior tibial tendon (PTT), which connects from your lower leg, along your ankle, to the middle of the arch, broken or dislocated bones. Some health conditions, such as rheumatoid arthritis, Nerve problems. Other factors that can increase your risk include obesity, diabetes, ageing and Pregnancy.
Symptoms
The primary symptom of flatfeet is the absence of an arch upon standing. Additional signs of flatfeet include the following. Foot pain. Pain or weakness in the lower legs. Pain or swelling on the inside of the ankle. Uneven shoe wear. While most cases of flatfeet do not cause problems, complications can sometimes occur. Complications include the following, bunions and calluses, inability to walk or run normally, inflammation and pain in the bottom of the foot (plantar fasciitis), tendonitis in the Achilles heel and other ligaments, pain in the ankles, knees, and hips due to improper alignment, shin splints, stress fractures in the lower legs.
Diagnosis
People who have flat feet without signs or symptoms that bother them do not generally have to see a doctor or podiatrist about them. However, if any of the following occur, you should see your GP or a podiatrist. The fallen arches (flat feet) have developed recently. You experience pain in your feet, ankles or lower limbs. Your unpleasant symptoms do not improve with supportive, well-fitted shoes. Either or both feet are becoming flatter. Your feet feel rigid (stiff). Your feet feel heavy and unwieldy. Most qualified health care professionals can diagnose flat feet just by watching the patient stand, walk and examining his/her feet. A doctor will also look at the patient's medical history. The feet will be observed from the front and back. The patient may be asked to stand on tip-toe while the doctor examines the shape and functioning of each foot. In some cases the physician may order an X-ray, CT (computed tomography) scan, or MRI (magnetic resonance imaging) scan.
Non Surgical Treatment
If you have flat feet and foot pain, especially if one foot is flatter than the other, you should have an evaluation by an orthopedic surgeon . You may have a problem with the posterior tibial tendon , the main tendon that supports the arch. Factors that can contribute to this problem are obesity, diabetes , high blood pressure , certain types of arthritis and athletic overuse. In some cases a shoe insert/orthotic can be used to alleviate the symptoms of flat feet.
Surgical Treatment

This is rare and usually only offered if patients have significant abnormalities in their bones or muscles. Treatments include joint fusion, reshaping the bones in the foot, and occasionally moving around tendons in the foot to help balance out the stresses (called tendon transfer).
Prevention
oll away pain. If you're feeling pain in the arch area, you can get some relief by massaging the bottom of your foot. A regular massage while you're watching TV can do wonders" Stretch out. Doing the same type of stretching exercises that runners do in their warm-up can help reduce arch pain caused by a tight heel cord. One of the best exercises is to stand about three feet from a wall and place your hands on the wall. Leaning toward the wall, bring one foot forward and bend the knee so that the calf muscles of the other leg stretch. Then switch legs. Stretching is particularly important for women who spend all week in heels and then wear exercise shoes or sneakers on weekends. Get measured each time you buy new shoes. Don't assume that since you always wore a particular size, you always will. Too many people try to squeeze into their 'regular' shoe size and wind up with serious foot problems or sores on their feet. When your arch is falling, your feet may get longer or wider and you may or may not feel pain, so getting your foot measured each time you buy shoes is a good indicator of your arch's degeneration. Examine your shoes. If the heel is worn down, replace it. But if the back portion of the shoe is distorted or bent to one side, get yourself into a new pair of supportive shoes like those made specifically for walking. That's because flat feet can affect your walking stride, and failing to replace worn shoes may lead to knee or hip pain.

 An Achilles tendon rupture is when you tear the tissue that connects your calf muscle to your heel bone. Your Achilles tendon is very strong and flexible. Its at the back of your ankle and connects your calf muscle to the bone in the heel of your foot (calcaneum). If you rupture your Achilles tendon, you can either partially or completely tear the tendon. Most people who injure their Achilles tendon are between 30 and 50 and dont exercise regularly. Its more common in men but can affect anyone. It happens most often in the left leg. This may be because most people are right-handed which means that they push off more frequently with the left foot when running.
An Achilles tendon rupture is when you tear the tissue that connects your calf muscle to your heel bone. Your Achilles tendon is very strong and flexible. Its at the back of your ankle and connects your calf muscle to the bone in the heel of your foot (calcaneum). If you rupture your Achilles tendon, you can either partially or completely tear the tendon. Most people who injure their Achilles tendon are between 30 and 50 and dont exercise regularly. Its more common in men but can affect anyone. It happens most often in the left leg. This may be because most people are right-handed which means that they push off more frequently with the left foot when running.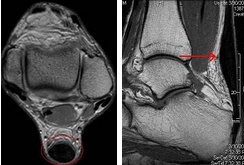
 RSS Feed
RSS Feed
