Overview

When standing, most people have a gap under the arch of their foot. Flat feet, or pes planus is the term used to describe collapsed arches, meaning that the entire sole of the foot rests partially or completely on the ground. A simple way to check to see if you have flat feet is to wet your feet and step onto a dry, flat surface. Step away from your footprint; if you see a complete footprint, you more than likely have flat feet. If you only see toes, the pads of your feet, and your heels, you probably do not have flat feet. People who have flat feet usually roll their feet over to the inner side when they walk. The feet may even appear to point outward because of this movement. In most cases, the condition cannot be prevented.
Causes
Fallen arches may be caused by a number of causes, including increased elastin during pregnancy, arthritis, injury, excessive stress on the foot, fused bones in the foot, or an extra bone. They may cause not only foot pain, but also pain in the legs, knees, and back and a loss of mobility. The condition is most often treated with orthotics, structures placed in the shoes to support the feet, but this may not be enough for severe cases. Exercises to strengthen and rebuild the arches can also be helpful. Surgery is sometimes the best method of treatment, as it can completely rebuild the arches and has lasting results, but it is quite expensive and considered a last resort.
Symptoms
Fallen arches symptoms may include the following. Being unable to slip fingers underneath arches. Inwards rolling of foot and ankle when running. Knee problems due to lack of support from feet.
Diagnosis
Runners are often advised to get a gait analysis to determine what type of foot they have and so what kind of running shoe they require. This shouldn?t stop at runners. Anyone that plays sports could benefit from this assessment. Sports shoes such as football boots, astro trainers and squash trainers often have very poor arch support and so for the 60-80% of us who do overpronate or have flat feet they are left unsupported. A change of footwear or the insertion of arch support insoles or orthotics can make a massive difference to your risk of injury, to general aches and pains and even to your performance.
best arch support insoles for flat feet
Non Surgical Treatment
Ligaments hold up arches. Deformed ligaments will not return to their original shape, just as an overstretched rubber band remains elongated. Arch supports help restore more normal function. Not all orthotics are made alike. Sole Supports custom designed orthotics are unique in the way they are cast. Sole Supports compensate for the differences between each foot. They take into account your body weight and the degree of flexibility in your feet. Taking care of fallen arches can be key in dealing with unresolved or recurrent back pain.
Surgical Treatment

A combination of surgical procedures can be used to reconstruct the flatfoot. Generally, these procedures can be separated into those that correct deformities of the bones and those that repair ligaments and tendons. Your orthopaedic surgeon will choose the proper combination of procedures for your foot. Surgery of the foot can be performed under regional anesthesia, which is numbing the foot and ankle with a nerve or spinal block, or general anesthesia, which may require a breathing tube. A nerve block is often placed behind the knee to reduce pain after surgery.
Prevention
oll away pain. If you're feeling pain in the arch area, you can get some relief by massaging the bottom of your foot. A regular massage while you're watching TV can do wonders" Stretch out. Doing the same type of stretching exercises that runners do in their warm-up can help reduce arch pain caused by a tight heel cord. One of the best exercises is to stand about three feet from a wall and place your hands on the wall. Leaning toward the wall, bring one foot forward and bend the knee so that the calf muscles of the other leg stretch. Then switch legs. Stretching is particularly important for women who spend all week in heels and then wear exercise shoes or sneakers on weekends. Get measured each time you buy new shoes. Don't assume that since you always wore a particular size, you always will. Too many people try to squeeze into their 'regular' shoe size and wind up with serious foot problems or sores on their feet. When your arch is falling, your feet may get longer or wider and you may or may not feel pain, so getting your foot measured each time you buy shoes is a good indicator of your arch's degeneration. Examine your shoes. If the heel is worn down, replace it. But if the back portion of the shoe is distorted or bent to one side, get yourself into a new pair of supportive shoes like those made specifically for walking. That's because flat feet can affect your walking stride, and failing to replace worn shoes may lead to knee or hip pain.
After Care
Time off work depends on the type of work as well as the surgical procedures performed. . A patient will be required to be non-weight bearing in a cast or splint and use crutches for four to twelve weeks. Usually a patient can return to work in one to two weeks if they are able to work while seated. If a person's job requires standing and walking, return to work may take several weeks. Complete recovery may take six months to a full year. Complications can occur as with all surgeries, but are minimized by strictly following your surgeon's post-operative instructions. The main complications include infection, bone that is slow to heal or does not heal, progression or reoccurrence of deformity, a stiff foot, and the need for further surgery. Many of the above complications can be avoided by only putting weight on the operative foot when allowed by your surgeon.

When standing, most people have a gap under the arch of their foot. Flat feet, or pes planus is the term used to describe collapsed arches, meaning that the entire sole of the foot rests partially or completely on the ground. A simple way to check to see if you have flat feet is to wet your feet and step onto a dry, flat surface. Step away from your footprint; if you see a complete footprint, you more than likely have flat feet. If you only see toes, the pads of your feet, and your heels, you probably do not have flat feet. People who have flat feet usually roll their feet over to the inner side when they walk. The feet may even appear to point outward because of this movement. In most cases, the condition cannot be prevented.
Causes
Fallen arches may be caused by a number of causes, including increased elastin during pregnancy, arthritis, injury, excessive stress on the foot, fused bones in the foot, or an extra bone. They may cause not only foot pain, but also pain in the legs, knees, and back and a loss of mobility. The condition is most often treated with orthotics, structures placed in the shoes to support the feet, but this may not be enough for severe cases. Exercises to strengthen and rebuild the arches can also be helpful. Surgery is sometimes the best method of treatment, as it can completely rebuild the arches and has lasting results, but it is quite expensive and considered a last resort.
Symptoms
Fallen arches symptoms may include the following. Being unable to slip fingers underneath arches. Inwards rolling of foot and ankle when running. Knee problems due to lack of support from feet.
Diagnosis
Runners are often advised to get a gait analysis to determine what type of foot they have and so what kind of running shoe they require. This shouldn?t stop at runners. Anyone that plays sports could benefit from this assessment. Sports shoes such as football boots, astro trainers and squash trainers often have very poor arch support and so for the 60-80% of us who do overpronate or have flat feet they are left unsupported. A change of footwear or the insertion of arch support insoles or orthotics can make a massive difference to your risk of injury, to general aches and pains and even to your performance.
best arch support insoles for flat feet
Non Surgical Treatment
Ligaments hold up arches. Deformed ligaments will not return to their original shape, just as an overstretched rubber band remains elongated. Arch supports help restore more normal function. Not all orthotics are made alike. Sole Supports custom designed orthotics are unique in the way they are cast. Sole Supports compensate for the differences between each foot. They take into account your body weight and the degree of flexibility in your feet. Taking care of fallen arches can be key in dealing with unresolved or recurrent back pain.
Surgical Treatment

A combination of surgical procedures can be used to reconstruct the flatfoot. Generally, these procedures can be separated into those that correct deformities of the bones and those that repair ligaments and tendons. Your orthopaedic surgeon will choose the proper combination of procedures for your foot. Surgery of the foot can be performed under regional anesthesia, which is numbing the foot and ankle with a nerve or spinal block, or general anesthesia, which may require a breathing tube. A nerve block is often placed behind the knee to reduce pain after surgery.
Prevention
oll away pain. If you're feeling pain in the arch area, you can get some relief by massaging the bottom of your foot. A regular massage while you're watching TV can do wonders" Stretch out. Doing the same type of stretching exercises that runners do in their warm-up can help reduce arch pain caused by a tight heel cord. One of the best exercises is to stand about three feet from a wall and place your hands on the wall. Leaning toward the wall, bring one foot forward and bend the knee so that the calf muscles of the other leg stretch. Then switch legs. Stretching is particularly important for women who spend all week in heels and then wear exercise shoes or sneakers on weekends. Get measured each time you buy new shoes. Don't assume that since you always wore a particular size, you always will. Too many people try to squeeze into their 'regular' shoe size and wind up with serious foot problems or sores on their feet. When your arch is falling, your feet may get longer or wider and you may or may not feel pain, so getting your foot measured each time you buy shoes is a good indicator of your arch's degeneration. Examine your shoes. If the heel is worn down, replace it. But if the back portion of the shoe is distorted or bent to one side, get yourself into a new pair of supportive shoes like those made specifically for walking. That's because flat feet can affect your walking stride, and failing to replace worn shoes may lead to knee or hip pain.
After Care
Time off work depends on the type of work as well as the surgical procedures performed. . A patient will be required to be non-weight bearing in a cast or splint and use crutches for four to twelve weeks. Usually a patient can return to work in one to two weeks if they are able to work while seated. If a person's job requires standing and walking, return to work may take several weeks. Complete recovery may take six months to a full year. Complications can occur as with all surgeries, but are minimized by strictly following your surgeon's post-operative instructions. The main complications include infection, bone that is slow to heal or does not heal, progression or reoccurrence of deformity, a stiff foot, and the need for further surgery. Many of the above complications can be avoided by only putting weight on the operative foot when allowed by your surgeon.




 Morton's neuroma is a swollen, inflamed nerve in the foot.Morton's neuroma causes a "burning" sharp pain on the bottom of the foot. Treatments for Morton's neuroma include resting the foot, better-fitting shoes, anti-inflammation medications, ice packs, and operation. A neuroma is growth (benign tumor) that arises in nerve cells. A Morton's neuroma is a swollen, inflamed nerve located between the bones at the ball of the foot. The most common location of a Morton's neuroma is in either the second or the third spacing from the base of the big toe.
Morton's neuroma is a swollen, inflamed nerve in the foot.Morton's neuroma causes a "burning" sharp pain on the bottom of the foot. Treatments for Morton's neuroma include resting the foot, better-fitting shoes, anti-inflammation medications, ice packs, and operation. A neuroma is growth (benign tumor) that arises in nerve cells. A Morton's neuroma is a swollen, inflamed nerve located between the bones at the ball of the foot. The most common location of a Morton's neuroma is in either the second or the third spacing from the base of the big toe.




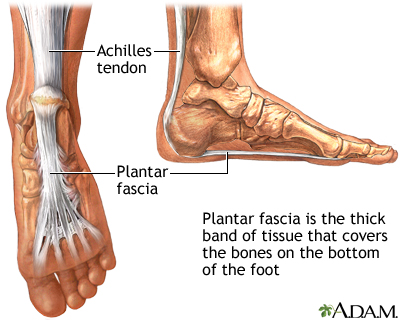

 The Achilles tendon connects your calf muscles to your heel bone. Together, they help you push your heel off the ground and go up on your toes. You use these muscles and your Achilles tendon when you walk, run, and jump. If your Achilles tendon stretches too far, it can tear or rupture. If this happens, you may hear a snapping, cracking, or popping sound and feel a sharp pain in the back of your leg or ankle. Have trouble moving your foot to walk or go up stairs. Have difficulty standing on your toes. Have bruising or swelling in your leg or foot. Causes The Achilles tendon usually ruptures as a result of a sudden forceful contraction of the calf muscles. Activities such as jumping, lunging, or sprinting can cause undue stress on the Achilles tendon and cause it to rupture. Often there is a background of Achilles tendinitis. Direct trauma to the area, poor flexibility or weakness of the calf muscles or of the Achilles tendon and increasing age are some of the other factors that are associated with an Achilles tendon rupture. Symptoms Tendon strain or tendon inflammation (tendonitis) can occur from tendon injury or overuse and can lead to a rupture. Call your doctor if you have signs of minor tendon problems. Minor tenderness and possible swelling increases with activity. There is usually no specific event causing sudden pain and no obvious gap in the tendon. You can still walk or stand on your toes. Acute calf pain and swelling can indicate a tear or partial tear of the Achilles tendon where it meets the calf muscle. You may still be able to use that foot to walk, but you will need to see a specialist such as an orthopedic surgeon. Surgery is not usually done for partial tears. Sometimes special heel pads or orthotics in your shoes may help. Follow up with your doctor to check for tendonitis or strain before resuming activity, because both can increase the risk of tendon rupture. Any acute injury causing pain, swelling, and difficulty with weight-bearing activities such as standing and walking may indicate you have a tear in your Achilles tendon. Seek prompt medical attention from your doctor or emergency department. Do not delay! Early treatment results in better outcome. If you have any question or uncertainty, get it checked. Diagnosis Most Achilles tendon ruptures occur in people between 30 and 50 years old and such injuries are often sport-related. If you suspect an Achilles injury, it is best to apply ice, elevate the leg, and see a specialist. One of the first things the doctor will do is evaluate your leg and ankle for swelling and discoloration. You may feel tenderness and the doctor may detect a gap where the ends of the tendon are separated. In addition to X-rays, the calf squeeze, or Thompson test, will be performed to confirm an Achilles tendon rupture. With your knee bent, the doctor will squeeze the muscles of your calf and if your tendon is intact the foot and ankle will automatically flex downward. In the case of a ruptured Achilles there will be no movement in the foot and ankle during the test. Non Surgical Treatment Non-surgical treatment typically involves wearing a brace or cast for the first six weeks following the injury to allow time for the ends of the torn tendon to reattach on their own. Over-the-counter medications, such as ibuprofen or aspirin, may be taken during this time to reduce pain and swelling. Once the tendon has reattached, physical therapy will be needed to strengthen the muscles and tendon. A full recovery is usually made within four to six months.
The Achilles tendon connects your calf muscles to your heel bone. Together, they help you push your heel off the ground and go up on your toes. You use these muscles and your Achilles tendon when you walk, run, and jump. If your Achilles tendon stretches too far, it can tear or rupture. If this happens, you may hear a snapping, cracking, or popping sound and feel a sharp pain in the back of your leg or ankle. Have trouble moving your foot to walk or go up stairs. Have difficulty standing on your toes. Have bruising or swelling in your leg or foot. Causes The Achilles tendon usually ruptures as a result of a sudden forceful contraction of the calf muscles. Activities such as jumping, lunging, or sprinting can cause undue stress on the Achilles tendon and cause it to rupture. Often there is a background of Achilles tendinitis. Direct trauma to the area, poor flexibility or weakness of the calf muscles or of the Achilles tendon and increasing age are some of the other factors that are associated with an Achilles tendon rupture. Symptoms Tendon strain or tendon inflammation (tendonitis) can occur from tendon injury or overuse and can lead to a rupture. Call your doctor if you have signs of minor tendon problems. Minor tenderness and possible swelling increases with activity. There is usually no specific event causing sudden pain and no obvious gap in the tendon. You can still walk or stand on your toes. Acute calf pain and swelling can indicate a tear or partial tear of the Achilles tendon where it meets the calf muscle. You may still be able to use that foot to walk, but you will need to see a specialist such as an orthopedic surgeon. Surgery is not usually done for partial tears. Sometimes special heel pads or orthotics in your shoes may help. Follow up with your doctor to check for tendonitis or strain before resuming activity, because both can increase the risk of tendon rupture. Any acute injury causing pain, swelling, and difficulty with weight-bearing activities such as standing and walking may indicate you have a tear in your Achilles tendon. Seek prompt medical attention from your doctor or emergency department. Do not delay! Early treatment results in better outcome. If you have any question or uncertainty, get it checked. Diagnosis Most Achilles tendon ruptures occur in people between 30 and 50 years old and such injuries are often sport-related. If you suspect an Achilles injury, it is best to apply ice, elevate the leg, and see a specialist. One of the first things the doctor will do is evaluate your leg and ankle for swelling and discoloration. You may feel tenderness and the doctor may detect a gap where the ends of the tendon are separated. In addition to X-rays, the calf squeeze, or Thompson test, will be performed to confirm an Achilles tendon rupture. With your knee bent, the doctor will squeeze the muscles of your calf and if your tendon is intact the foot and ankle will automatically flex downward. In the case of a ruptured Achilles there will be no movement in the foot and ankle during the test. Non Surgical Treatment Non-surgical treatment typically involves wearing a brace or cast for the first six weeks following the injury to allow time for the ends of the torn tendon to reattach on their own. Over-the-counter medications, such as ibuprofen or aspirin, may be taken during this time to reduce pain and swelling. Once the tendon has reattached, physical therapy will be needed to strengthen the muscles and tendon. A full recovery is usually made within four to six months.  Surgical Treatment Surgery is recommended to those who are young to middle-aged and active. The ruptured tendon is sewn together during surgery. This is an outpatient procedure. Afterward the leg is put into a splint cast or walking boot. Physical therapy will be recommended. In about 4 to 6 months, healing is nearly complete. However, it can take up to a year to return to sports fully.
Surgical Treatment Surgery is recommended to those who are young to middle-aged and active. The ruptured tendon is sewn together during surgery. This is an outpatient procedure. Afterward the leg is put into a splint cast or walking boot. Physical therapy will be recommended. In about 4 to 6 months, healing is nearly complete. However, it can take up to a year to return to sports fully.
 Achilles tendinitis is a common condition that causes pain along the back of the leg near the heel. The Achilles tendon is the largest tendon in the body. It connects your calf muscles to your heel bone and is used when you walk, run, and jump. Although the Achilles tendon can withstand great stresses from running and jumping, it is also prone to tendinitis, a condition associated with overuse and degeneration. Simply defined, tendinitis is inflammation of a tendon. Inflammation is the body's natural response to injury or disease, and often causes swelling, pain, or irritation. There are two types of Achilles tendinitis, based upon which part of the tendon is inflamed. Noninsertional Achilles tendinitis, Noninsertional Achilles Tendinitis. In noninsertional In both noninsertional and insertional Achilles tendinitis, damaged tendon fibers may also calcify (harden). Tendinitis that affects the insertion of the tendon can occur at any time, even in patients who are not active.
Achilles tendinitis is a common condition that causes pain along the back of the leg near the heel. The Achilles tendon is the largest tendon in the body. It connects your calf muscles to your heel bone and is used when you walk, run, and jump. Although the Achilles tendon can withstand great stresses from running and jumping, it is also prone to tendinitis, a condition associated with overuse and degeneration. Simply defined, tendinitis is inflammation of a tendon. Inflammation is the body's natural response to injury or disease, and often causes swelling, pain, or irritation. There are two types of Achilles tendinitis, based upon which part of the tendon is inflamed. Noninsertional Achilles tendinitis, Noninsertional Achilles Tendinitis. In noninsertional In both noninsertional and insertional Achilles tendinitis, damaged tendon fibers may also calcify (harden). Tendinitis that affects the insertion of the tendon can occur at any time, even in patients who are not active.
 RSS Feed
RSS Feed
